Vaccine shortages at Toronto pop-up clinics are leaving many residents in the city’s hot-spot postal codes unable to secure a COVID-19 vaccine and disheartened by their prospects at getting one.

Vaccine shortages at Toronto pop-up clinics are leaving many residents in the city’s hot-spot postal codes unable to secure a COVID-19 vaccine and disheartened by their prospects at getting one.
“We’re frustrated; we don’t know where to go,” Lorraine Lendor, a kindergarten teacher who unsuccessfully tried to get a vaccine on Saturday, told CBC News.
The Ontario government has said it would prioritize vaccines in Toronto’s hardest-hit, lower-income areas, with health units now offering pop-up vaccination clinics in those neighbourhoods for people aged 18 and older.
However, some residents said they’ve waited in line for hours just to be turned away.
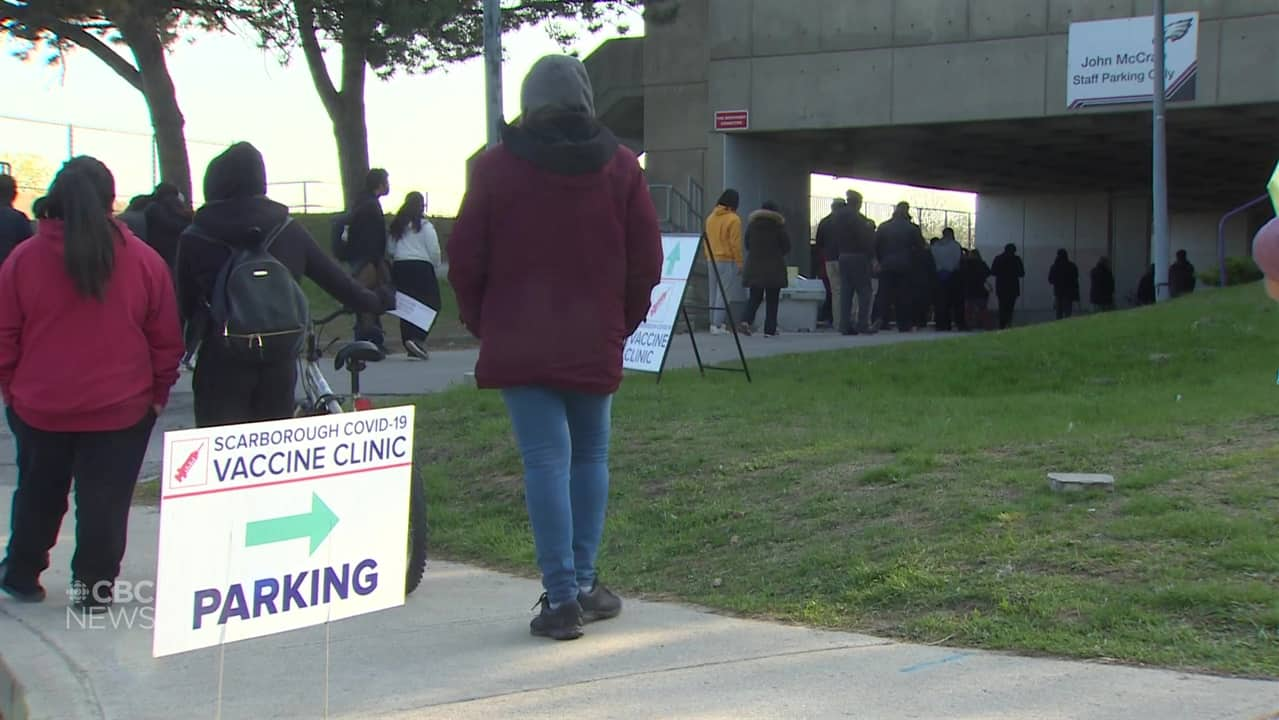
Ashak Rahman, who was in line at a pop-up clinic at John McCrae Public School in Scarborough on Saturday, said it was his second day in a row attempting to get a COVID-19 vaccine.
“I came here yesterday as well, but I couldn’t get the appointment,” he told CBC News while waiting in line.
WATCH | Hundreds in COVID-19 hot spots frustrated by pop-up clinics:
The province has set up vaccine clinics for people living in areas hit hard by the pandemic, but there are growing concerns about who has access and how they’re getting it. CBC’s Jessica Ng has the story. 2:41
Lendor said she arrived at the same pop-up clinic in her Scarborough neighbourhood at 7 a.m. ET on Saturday in hopes of getting vaccinated. She previously had an appointment booked through the provincial booking portal, but said it was cancelled due to lack of vaccine supply.
Despite showing up three hours before the pop-up clinic at the public school opened, Lendor said there was already a line stretching five blocks — with hundreds of people crowding to the site over the hours.
At one point, she said nurses from the clinic told people in line that the clinic ran out of vaccines and those still in line would have to come back another day.
“I’m back to square one,” Lendor said, “And if I have to do a pop-up again, I feel like I might have to sleep in my car and just wait.”
‘What I saw today, that should have never happened’
According to recent data from the Institute for Clinical Evaluative Sciences (ICES), the disparity between COVID-19 vaccination rates in hot spots and those in affluent areas is levelling off.
But the independent, non-profit corporation that conducts health research in Ontario said many areas facing highest rates of transmission of the virus still have much lower vaccination rates than more affluent neighbourhoods.
“It’s getting to be more similar — but I think the highest risk areas are still lagging a bit,” Jeff Kwong, senior scientist at ICES, said on Friday.
Lendor said hot-spot areas like her M1J postal code should have more than one pop-up clinic in order to accommodate everyone.
“There was no way that this clinic was going to do that,” she said. “What I saw today, that should have never happened.”
Rouf Abdur, another person who was turned away at the pop-up clinic outside the public school, questioned why there were such limited vaccines at the location when the postal code is home to almost 40,000 people. He said the location offered about 1,000 doses.
“At least 5,000 vaccines should be here,” he said.
Dr. Naheed Dosani, a palliative care physician and health justice activist, questioned whether these clinics have enough supply to vaccinate people in these at-risk areas.
“We’re learning that these mobile vaccine programs may not even have the supply to vaccinate people. This really doesn’t bode well if this is our only strategy to connect with hard-hit communities,” he said.
Dosani said a strategy that involves adequate supply of vaccines for pop-up and mobile clinics and more communication with these hard-hit communities is required to protect those most at risk for COVID-19.

In a statement to CBC News, a spokesperson for Ontario’s Ministry of Health said the province is dedicating 25 per cent of future vaccine allocations to 13 public health regions that need it most.
But Dosani said the way pop-up vaccine clinics are structured doesn’t address transmission in those areas. He said factors like income, precarious employment and multi-generational households are factors that are driving further COVID-19 infections in hot spots.
The lineups in Scarborough are a reminder that racialized & low-income communities want vaccines. They just lack access because of an inequitable vaccine rollout.
✖️ Vaccine hesitant
✅ Vaccine confident + limited access
Reallocate vaccines to hotspots or people will die. pic.twitter.com/jxlDSef7HQ
—@NaheedD
Science table suggests hot-spot-targeted vaccine strategy
On Friday, Ontario’s COVID-19 science table released a report that recommended a shift in the province’s vaccine strategy, which would see the allocation of vaccines based on transmission rate instead of age cohort.
The report said this “hot-spot-accelerated strategy” would significantly reduce COVID-19 case counts, hospitalizations and deaths.
The group of scientific experts and health system leaders said early analysis shows residents of neighbourhoods with the lowest risk of COVID-19 are 1.5 times more likely to have received at least one dose of the vaccine.
Dr. Peter Jüni, the table’s director, said this strategy will indirectly protect more Ontario residents by directly protecting those most severely affected.
“If we go with a lot of our vaccines into those neighbourhoods in Ontario who are most severely affected by COVID-19 and have a lot of essential workers and their families living there, then what we see is that the strategy […] benefits everybody in the province,” he told CBC News Network on Saturday.
